CAR-T cell therapy
In addition to surgery, chemotherapy, targeted therapy, radiotherapy, a new way of fighting cancer has recently become available. It is CAR-T cell therapy, where CAR stands for chimeric antigen receptor, and T cells are cells of the patient’s own immune system.
A new chance
One of the most important ideas in present-day oncology is the idea that we should use the body’s own immune system to fight cancer cells. But, evidently, the power of the immune system alone is normally insufficient for this purpose (otherwise, cancer would not develop!), and it needs one or another kind of stimulation, one or another way of purposely directing it toward cancer cells. CAR-T cell therapy is exactly such a way, and there have already been many examples of its successful use.
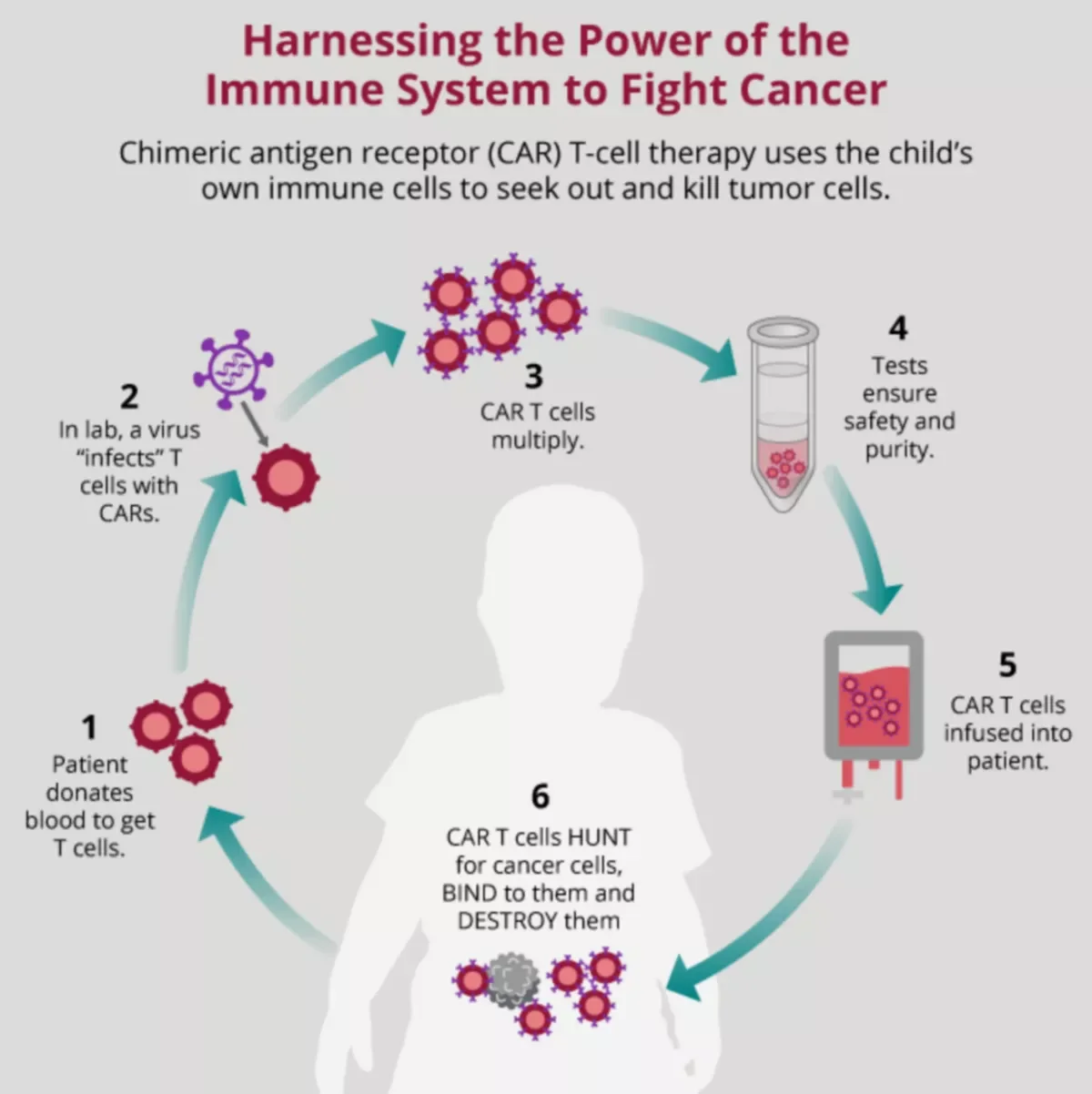
Actually, it is not just a therapy but a technology, where the cell product is prepared individually for every patient. First, the patient’s own immune cells (T cells) are taken. Then, they are genetically modified in the laboratory so that they “learn” to target the cancer cells — that is when they acquire the CAR, that is, the chimeric antigen receptor. Afterward, these modified cells are infused back into the patient’s bloodstream and start their fight. In children with acute leukemia, CAR-T therapy is often used in combination with bone marrow transplantation, in cases when the transplantation alone would not be enough.
CAR-T therapy involves complex high-tech procedures, which are still available in only a limited number of medical centers. It requires skilled physicians and special laboratory reagents. It is associated with a significant risk of complications. And it is still used only in the most difficult cases, where all other treatments have failed. However, in these cases it often creates wonders: many people who have already lost hope may actually be saved.
Unfortunately, making CAR-T cell therapy work for solid tumors is a still unsolved problem. However, it can be very efficient in blood cancers. B-cell acute lymphoblastic leukemia, diffuse large B-cell lymphoma, multiple myeloma, acute myeloid leukemia… Year after year, new targets for this therapy are being tested around the world, and year after year, new lives are saved.
CAR T-cell therapy is expensive. For example, treatment with Kymriah or Yescarta, the first such therapies approved by the FDA, costs several hundred thousand dollars. Similar technologies available in other countries are much cheaper, but still there may be serious associated expenses, such as the cost of reagents, hospitalization, treatment for complications, and so on and for many children with leukemia it is the only chance.